FDA Lessons: Avoiding Common Cleaning Validation Pitfalls
Staying ahead of FDA scrutiny demands more than basic compliance—it requires a proactive, risk-based Cleaning Validation Protocol strategy. Many pharma manufacturers continue to receive FDA 483s and warning letters for avoidable gaps in their cleaning validation process. Addressing these pitfalls with scientific rigor, advanced documentation, and digital automation is mission-critical for QA, QC, and validation professionals.
Why Cleaning Validation Pitfalls Are Still Costing Pharma Companies
The Regulatory Reality
Recent FDA inspections reveal that cleaning validation remains a primary focus area, especially where multi-product manufacturing and shared equipment heighten risk. Observations highlight protocol lapses, incomplete studies, and documentation issues that lead to non-compliance and costly remediation efforts.
Pro Tip: Stop repeat FDA 483 findings by automating audit trails, revalidation triggers, and documentation with Leucine’s Cleaning Validation Software (CLEEN).
The Most Common FDA Cleaning Validation Pitfalls (and How to Avoid Them)
- Incomplete or Outdated Cleaning Validation Protocols
- What the FDA Finds: Protocols lacking detailed procedures, sampling methods, acceptance criteria, or up-to-date risk-based rationale.
- How to Avoid: Standardize and regularly update your Cleaning Validation Protocol to reflect process changes and the latest cGMP expectations. Include scientifically justified limits and robust rationales.
- Unscientific or Undefined Acceptance Criteria
- Pitfall: Overreliance on visual inspection or arbitrary residue thresholds.
- How to Avoid: Implement scientifically justified residue limits using HBELs, MACO, and product-specific calculations. Always include worst-case scenarios in your validation design.
- Insufficient or Non-Validated Analytical Methods
- Pitfall: Relying on unvalidated swab, rinse, or TOC methods; failing to define low-solubility or high-toxicity product risks.
- How to Avoid: Validate all analytical methods for detection, specificity, and recovery. Use a combination of swab sampling, TOC analysis, and rinse samples for robust verification.
- Poor Documentation and Change Control
- Pitfall: Missing, illegible, or inconsistent records; gaps after process or equipment changes.
- How to Avoid: Use digital, version-controlled documentation; link every protocol update, deviation, and corrective action in a central audit portal like CLEEN. Implement strict change management workflows.
- Lack of Lifecycle Management and Monitoring
- Pitfall: Treating validation as a one-time event without routine monitoring, trend analysis, or scheduled revalidation.
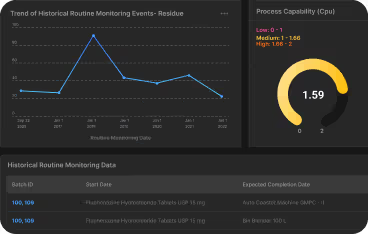
- How to Avoid: Integrate continuous monitoring, data trending, and trigger-based revalidation into your cleaning validation lifecycle. Learn more in the Audit Readiness Checklist 2025.
- Operator Training and Execution Gaps
- Pitfall: Inadequate training leads to SOP deviations and inconsistent cleaning outcomes.
- How to Avoid: Maintain robust, role-specific training records and ensure only trained personnel execute and document cleaning validation steps. Explore compliance SOP best practices →
How Automated Solutions Help Avoid FDA Pitfalls
Leucine CLEEN delivers:
- Automated protocol management, risk assessment, and documentation
- Instant residue calculations and data integration from LIMS for real-time compliance
- Audit-ready reports, digital audit trail, and standard templates that align with global (FDA, EMA, WHO) requirements
- Configurable alerts for revalidation and deviation investigation triggers
Pro Tip: Let CLEEN flag missing data, trigger revalidation after changes, and maintain a single source of truth for all cleaning validation activities—minimizing human error and inspection delays.
Best Practices for Staying FDA Audit-Ready
- Adopt a risk-based approach: Focus on worst-case product and equipment combinations.
- Validate every method and sampling strategy: Use TOC, swab, and rinse sampling, all with proper recovery studies.
- Digitize your documentation: Move away from spreadsheets and paper—invest in solutions like CLEEN for version control, automated trending, and audit logs.
- Regularly schedule internal audits and training refreshers: Maintain up-to-date, role-specific training documentation.
Learn more about: Audit Readiness Checklist 2025 Cleaning Validation
Frequently Asked Questions
1. What is the number one cause of FDA 483 findings in cleaning validation?
The most common root cause is incomplete or poorly justified cleaning validation protocols—especially lacking scientific rationale, risk assessments, and robust documentation.
2. Is visual inspection alone acceptable for cleaning validation?
No, the FDA and EMA require quantitative, scientifically justified residue limits determined via validated analytical methods—visual checks serve only as supplementary measures.
3. How does automation mitigate cleaning validation pitfalls?
Automation ensures consistency, data integrity, and a comprehensive audit trail—reducing manual documentation errors and catching protocol gaps before they’re flagged by regulators.